Oral Health
4 min read
Aug 07, 2025
Signs You Might Have a Bacterial Infection in Your Jaw
Jaw pain might seem like a minor issue at first, but it can sometimes point to something far more serious, a bacterial infection deep within the bone. These infections can develop quickly and become dangerous if left untreated. Understanding the early warning signs is crucial for protecting your health and avoiding complications.

It starts off as a little jaw pain. You ignore it. Maybe it’s just from clenching your teeth too much or sleeping funny. But then it lingers… and worsens. Suddenly, you’re Googling symptoms at 2 AM with an ice pack pressed to your cheek. Sound familiar?
Here’s the truth: pain in your jaw, especially near a tooth or your jawbone, might not be something to brush off. It could be a sign of a bacterial infection in the jaw. And while that might sound dramatic, infection and inflammation in this area can get serious, fast.
Let’s break down the signs, what causes them, and what to do before it gets worse.
How a Jaw Infection Starts
Your mouth is often teeming with bacteria (don’t panic, that’s normal). But when bacteria sneak past your gum line, maybe through a cavity, cracked tooth, or untreated dental abscess, they can travel deeper into the jawbone. If they reach the bone tissue, that’s when things escalate.
A jaw infection, especially one caused by a bacterial infection, doesn’t just stay put. It can spread into the soft tissue, pulp of the tooth, or even beyond the tissues of the face and neck. That’s when we enter the danger zone of osteomyelitis of the jaw.
Common Risk Factors for Jaw Bone Infections
Let’s talk about risk factors, because knowing what puts you in the danger zone can help you avoid it. You might be more likely to develop an infection in the jaw if:
You’ve had recent tooth extraction, oral surgery, or root canal treatment
You have poor oral hygiene
You’re dealing with tooth decay or an untreated dental abscess
You smoke or have a weakened immune system
You’ve had trauma to the jaw bone
Even something like dry mouth can up your risk, since saliva plays a big role in washing away harmful bacteria.
Tooth Trouble That Signals Infection
That nagging tooth you’ve been avoiding? It could be more than just a nuisance. A tooth abscess (aka an abscessed tooth) is a big red flag. An abscess is a pocket of pus that forms due to an infected pulp, and if left untreated, it can spread straight into your jaw.
Symptoms include fever, swelling in the face and neck, a throbbing pain that radiates through your head and neck, and in some cases, visible pus. If your tooth may be loose or sensitive to touch, you should see a dentist right away. These are not things to sleep on.
What a Jaw Bone Infection Feels Like
Jaw osteomyelitis is no joke. This is a serious bone infection, and it doesn’t play nice. Osteomyelitis symptoms include:
Persistent jaw pain
Swelling in the affected area
Redness or warmth over the jaw
Fever, chills, or feeling generally lousy
Numbness or tingling in the jaw or face
Difficulty opening your mouth
In severe cases, you might even notice dead bone tissue (yep, that’s as scary as it sounds) or draining pus. That could mean the infection has spread.
Why Osteomyelitis of the Jaw Is So Serious
Still thinking you’ll just wait it out? Not a great plan. Chronic osteomyelitis of the jaw is rare, but it happens, and it can lead to serious, even life-threatening, complications. Once the infection may hit the jaw bone, it becomes harder to treat and may require debridement, bone grafting, or even removal of part of the jaw bone.
In some cases, a bone biopsy is needed to figure out exactly what type of bacteria we’re dealing with. It’s often streptococci and anaerobic bacteria, the usual troublemakers in dental infections.
When to Call the Dentist
If you develop symptoms include pain, swelling, or pus near a tooth or your jaw, don’t wait. Seek immediate help from a dentist. They’ll likely take X-rays or scans to check for lesion, bone loss, or signs of osteomyelitis.
If a tooth may need to be pulled or treated, they’ll walk you through your treatment options. Often, the dentist will try to drain the abscess, clean out the infected pulp, and prescribe antibiotic therapy.
Antibiotic Treatment and What to Expect
Depending on how far the infection may have spread, antibiotics may be prescribed for 7 to 14 days, sometimes longer. You’ll need to follow the full course of antibiotics, even if you start feeling better.
In some situations, antibiotic treatment alone isn’t enough. Oral surgery may be needed to rid of the infection, especially if there’s already damage to bone tissue. But don’t panic, early diagnosis usually means less invasive steps and a much smoother recovery.
How to Protect Your Jaw with Good Dental Care
Most dental infections promptly treated don’t turn into jaw nightmares. The best way to avoid all of this? Good oral hygiene and regular checkups.
Here’s your no-nonsense prevention plan:
Brush and floss daily
See your dentist at least twice a year
Don’t ignore cavity, gum, or tooth pain
Get that affected tooth looked at instead of toughing it out
Follow through on prompt treatment if something’s off
Your oral hygiene is the frontline defense against dangerous bacterial infections and bone infections. And hey, your smile will thank you too.
What Are the Common Signs of a Jaw Bone Infection?
Symptoms of a bacterial jaw infection often include persistent jaw pain, swelling, redness or warmth in the area, difficulty opening your mouth, and sometimes a fever. You may also notice numbness in the jaw or draining pus. These are red flags that need prompt dental evaluation.
How Does a Jaw Infection Usually Start?
A jaw infection often begins when bacteria from an untreated cavity, cracked tooth, or dental abscess enter deeper tissue or bone. This can happen after oral surgery, tooth extraction, or if poor oral hygiene allows bacteria to spread beneath the gumline.
When Should I See a Dentist About Jaw Pain?
You should call your dentist if you have jaw pain that worsens over time, swelling that doesn’t go down, visible pus, a loose tooth, or any symptoms of infection like fever or facial numbness. Early treatment helps prevent serious complications like osteomyelitis.
Can Antibiotics Alone Cure a Jaw Infection?
Antibiotics are often the first line of treatment and can clear up mild infections if taken correctly. However, more advanced cases, especially those involving bone, may require surgical intervention to remove infected tissue or drain an abscess. Early diagnosis increases the chance of avoiding surgery.
Read Next
Related Posts

Oral Health
Tooth Replacement Options to Prevent Bone Loss
Losing a tooth isn’t just about appearance, it can have a lasting impact on your oral health, jawbone strength, and overall quality of life. When teeth go missing, the jawbone begins to shrink, which can change your bite, your facial structure, and even your confidence. Fortunately, modern dentistry offers several effective solutions to replace missing teeth and prevent further bone loss.
4 min read
Sep 26, 2025
Oral Health
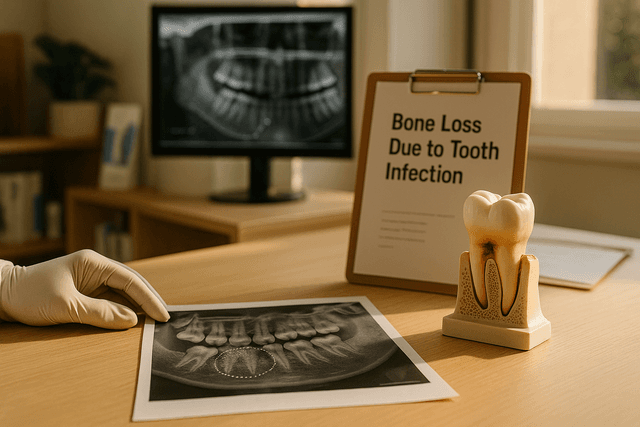
Bone Loss Due to Tooth Infection Explained: What It Means for Your Oral Health
A tooth infection isn’t just about pain, it can quietly damage the tissues around a tooth and even erode the jawbone that supports your smile. This guide explains how infections start, why they can lead to bone loss, the warning signs to watch for, and the treatments that can stop the spread and rebuild lost support.
5 min read
Sep 25, 2025

Oral Health
Understanding Bone Loss in Teeth: Causes and Treatments That Work
Bone loss in teeth is a silent threat that can compromise your smile, facial structure, and overall oral health. While it often goes unnoticed in the early stages, it can lead to serious consequences if left untreated. Understanding what causes dental bone loss, and how to prevent or manage it, is key to maintaining a strong, healthy foundation for your teeth.
5 min read
Sep 25, 2025
Don’t have time to research every dentist around you?
See why 30k+ patients trusted us