Oral Health
7 min read
Aug 19, 2024
Gum Disease Demystified: Causes, Symptoms, and Treatment
Unravel the mysteries of gum disease, understand its origins, symptoms, and explore effective treatment options for a healthy smile.

Let’s Talk About Gums
You probably don’t spend much time thinking about your gums, until they start acting up. Maybe they’re red, a little puffy, or you spotted blood on your floss. It’s easy to shrug it off. But that soft pink border around your teeth is more important than it gets credit for. Healthy gum tissue holds everything together. When it gets irritated or infected, you’re not just dealing with an annoying issue. You’re risking your smile, your comfort, and your overall health.
Understanding Gum Disease
Gum disease isn’t some faraway dental condition that only happens to unlucky folks. It’s common. Really common. According to the American Dental Association, a majority of adults will experience some form of gum disease during their lives. It starts quietly, maybe a little gum irritation when you brush, but left untreated, it can progress into a serious infection.
Also called gum disease, periodontal disease refers to infections that affect the structures around the teeth and gums. That includes the gum line, the soft tissues, and even the bone holding your teeth in place. When things get out of balance, harmful bacteria move in, and that's when the trouble begins.
The Trouble With Periodontitis
Now let’s get to the serious stuff. Periodontitis is the advanced stage of gum disease. It’s what happens when early warning signs go ignored and the infection digs deeper. At this point, it’s not just about sore gums. Periodontitis can damage the tissue and bone that support your teeth, causing them to become loose, or worse, fall out.
The symptoms of periodontitis aren’t always dramatic at first. A little bad breath. Some swelling. But as it progresses, you might notice your gum line receding, teeth shifting, or spaces forming where there weren’t any. The treatment of periodontitis often includes deep cleanings like scaling and root planing, and in more severe cases, gum graft surgery or other surgical options.
The Mild Menace of Gingivitis
Gingivitis is the mildest form of gum disease, and the easiest to ignore. Gums might look a bit red or swell slightly. You might notice bleeding when you brush or floss. That’s it. No pain. No major drama. But don’t let the mild symptoms fool you.
The biggest thing to know? Gingivitis can be reversed. With consistent brushing, flossing, and regular dental checkups, your gums can bounce back. But let it slide, and it could snowball into full-blown periodontitis. Gingivitis and periodontitis may sound like mouthfuls, but they’re two points on the same spectrum of disease, and you really don’t want to let things slide past the first stage.
Risk Factor Reality Check
Why do some people get gum disease while others seem to glide by with perfect gums? It comes down to a combination of risk factors. Some you can control, others not so much. Poor oral hygiene tops the list, if you skip flossing or brush inconsistently, plaque builds up fast. And plaque is sticky, relentless, and packed with bacteria.
Other risk factors for gum disease include smoking, a high-sugar diet, genetics, hormonal changes (especially during pregnancy), and certain health conditions like diabetes. People with diabetes are more likely to get gum disease and may have a harder time healing from it.
Even stress plays a role. It weakens your immune system, giving bacteria more room to thrive. Being aware of your risk factors makes it easier to spot issues early and get ahead of them.
What Is Periodontal Disease, Anyway?
Periodontal disease refers to the inflammation and infection of the gum and bone structure supporting your teeth. It’s not a single moment of dental disaster, it’s a slow-building issue. Over time, the bacteria in plaque irritate the gums, break down the tissue, and eventually attack the bone.
When tartar (hardened plaque) forms and isn’t removed during regular general dentistry visits, the infection can creep under the gum line. This stage of gum disease is where things can get dicey. The American Academy of Periodontology explains that periodontal disease can also affect your overall health, increasing risks of heart problems like coronary artery disease.
The Dentist Isn’t the Villain, They’re Your Ally
We get it, nobody’s thrilled to see a dentist. But your dentist isn’t just there for cavities and x-rays. They’re often the first to spot gum disease before it becomes painful or complicated. At your checkup, they may measure the depth of the spaces around your teeth using a tool called a periodontal probe. This helps diagnose how far the infection has progressed.
If they notice something off, they might refer you to a gum specialist known as a periodontist. Periodontists handle more advanced cases, offering professional treatment that goes beyond standard cleanings, like root planing, gum surgery, and targeted antibiotic therapies.
When to See a Dentist (Hint: Before It Hurts)
Here’s the kicker: gum disease doesn’t usually hurt until it’s already done some damage. That’s why it’s crucial to spot the warning signs. Signs of gum disease include bleeding gums, persistent bad breath, gums that pull away from teeth, or a change in how your teeth fit together when you bite.
If you experience any of these, don’t wait. See a dentist. If you don’t already have one, it’s worth learning how to choose a family dentist who can keep tabs on your gum health.
Gum Disease Symptoms to Watch Out For
Let’s lay it out. The symptoms of gum disease include:
Bleeding while brushing or flossing
Red or purplish gums
Swelling of the gum around the teeth
Gum tenderness or pain
Persistent bad breath
Gums pulling away from teeth
Teeth that feel loose
Changes in bite
If you're unsure whether the pain stems from gum disease or something else, explore toothache causes and remedies for clarity. These aren’t just cosmetic problems. They’re red flags that your oral health is at risk.
Dental Tools and Tips That Make a Difference
Regular dental visits matter, but what you do at home matters even more. Brushing twice a day (gently, please) and using fluoride toothpaste is a good start. Flossing daily helps remove plaque from areas your brush can’t reach. And if floss isn’t your thing, try a water flosser or interdental brush.
Seeing a dental hygienist regularly is key. They’re trained to spot the subtle signs of gum irritation, remove tartar, and teach you how to keep your teeth and gums clean between visits. Practices offering walk-in dentistry can make it easier to stay consistent with cleanings. It’s a team effort, and you’re the MVP.
Why Oral Health Is Bigger Than Just Teeth
You might think gum disease lives only in your mouth, but studies suggest a link between oral health and other health conditions. Infections in the mouth can send inflammatory signals through your bloodstream, potentially affecting your heart, lungs, and even blood sugar levels. Keeping your gums healthy means doing a favor for the rest of your body too.
Breaking Down the Stages of Gum Disease
Gum disease typically progresses through three stages:
Gingivitis: The mildest form of periodontal disease. Gums may bleed, swell, or feel tender. Gingivitis can be reversed with good oral care.
Moderate Periodontitis: Infection spreads deeper. You may notice your gums receding, forming pockets around the teeth.
Advanced Periodontitis: Severe gum and bone damage. Teeth may become loose and tooth loss becomes a real risk.
Without treatment, each stage worsens the next.
How to Prevent Gum Disease
Good news, gum disease is largely preventable. Here’s how:
Brush your teeth at least twice daily
Floss once a day (seriously, don’t skip this)
Avoid smoking or vaping
Eat a balanced diet with limited sugar
Schedule regular dental checkups and cleanings
Treat underlying health conditions like diabetes
Prevent gum disease by turning these into daily habits. Small changes make a big difference.
The Treatment Plan: From Scaling to Surgery
If you already have symptoms, don’t panic. Treatment of gum disease depends on the severity. In mild cases, a thorough cleaning and a little coaching from your dentist may be all you need.
More advanced stages might require deep cleaning, a deep-cleaning technique to remove plaque and tartar from below the gum line. In extreme cases, tooth extraction or gum graft surgery may be necessary to restore damaged gum tissue and bone.
A periodontist will build a personalized treatment plan based on how far the disease has progressed. With the right care, even severe gum disease can be managed, and your smile saved.
Gum Disease Can Cause More Than Just Bad Breath
This disease is an infection. It’s not just about bleeding when you floss or a little puffiness. Gum disease can cause tooth loss, bone loss, and complications that extend beyond the mouth. It’s one of the leading causes of tooth loss in adults. But it doesn’t have to go that far.
Let’s Wrap It Up (But Keep the Floss Handy)
The truth is, gum disease is sneaky. It builds over time, often without pain, until the damage is done. But with awareness, good oral hygiene, and regular dental care, you can stay ahead of it.
If you notice warning signs, don’t brush them off, literally or figuratively. Treatment can help, and professional treatment and good home care go hand-in-hand. You’ve got one set of teeth and gums. Keep them healthy, keep them strong, and don’t let gum disease steal your smile.
For more gum disease information or help creating a treatment plan tailored to you, trust your dentist or periodontist. They’re in your corner, and your gums will thank you.
What Are the Early Signs of Gum Disease?
Early signs of gum disease include red, swollen gums, bleeding when brushing or flossing, and persistent bad breath. These symptoms are often painless but signal inflammation caused by plaque buildup. Catching gum disease at this stage, known as gingivitis, allows for easy reversal with improved oral hygiene and regular dental cleanings.
How Serious Is Periodontitis Compared to Gingivitis?
Periodontitis is a more advanced and serious form of gum disease. While gingivitis affects only the surface of the gums, periodontitis damages the deeper tissues and bone that support your teeth. It can lead to gum recession, loose teeth, and even tooth loss if left untreated. Treatment may involve deep cleaning, medication, or gum surgery.
Can Gum Disease Affect Your Overall Health?
Yes, gum disease is linked to several systemic health conditions. The bacteria and inflammation associated with periodontal disease can enter the bloodstream, contributing to heart disease, diabetes complications, and respiratory issues. Keeping your gums healthy helps protect your overall well-being.
What’s the Best Way to Prevent Gum Disease?
Preventing gum disease starts with consistent oral care: brush twice daily, floss once a day, and avoid tobacco use. Eat a balanced diet low in sugar, manage stress, and visit your dentist regularly for cleanings and exams. Early intervention is key to keeping your gums and teeth healthy.
Read Next
Related Posts

Oral Health
Tooth Replacement Options to Prevent Bone Loss
Losing a tooth isn’t just about appearance, it can have a lasting impact on your oral health, jawbone strength, and overall quality of life. When teeth go missing, the jawbone begins to shrink, which can change your bite, your facial structure, and even your confidence. Fortunately, modern dentistry offers several effective solutions to replace missing teeth and prevent further bone loss.
4 min read
Sep 26, 2025
Oral Health
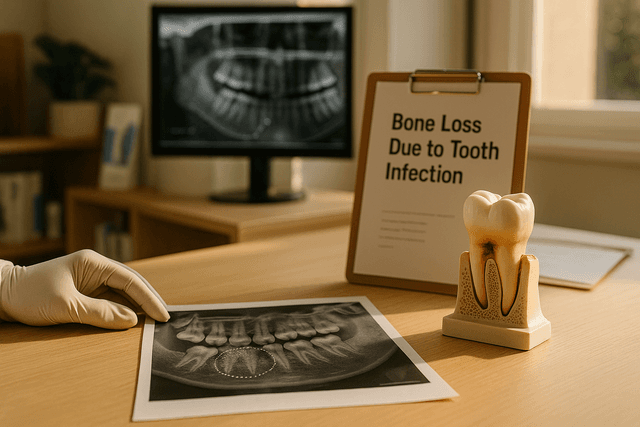
Bone Loss Due to Tooth Infection Explained: What It Means for Your Oral Health
A tooth infection isn’t just about pain, it can quietly damage the tissues around a tooth and even erode the jawbone that supports your smile. This guide explains how infections start, why they can lead to bone loss, the warning signs to watch for, and the treatments that can stop the spread and rebuild lost support.
5 min read
Sep 25, 2025

Oral Health
Understanding Bone Loss in Teeth: Causes and Treatments That Work
Bone loss in teeth is a silent threat that can compromise your smile, facial structure, and overall oral health. While it often goes unnoticed in the early stages, it can lead to serious consequences if left untreated. Understanding what causes dental bone loss, and how to prevent or manage it, is key to maintaining a strong, healthy foundation for your teeth.
5 min read
Sep 25, 2025
Don’t have time to research every dentist around you?
See why 30k+ patients trusted us