Prosthodontics
5 min read
Mar 28, 2025
Dental Implant Procedure: Step-by-Step Timeline (With Recovery Tips)
Dental implants replace missing teeth with artificial roots and crowns that look and function like natural teeth. They’re used to restore chewing ability, prevent jawbone loss, and improve facial structure. Unlike bridges or dentures, implants are surgically anchored into the jaw and designed to last for decades.

Getting a dental implant isn’t something you decide over lunch. If you're here, you've probably been living with a missing tooth, or a few, and you're ready to fix it for good. You've looked into your options, maybe even tried a denture or bridge, but you're looking for something that feels... real. Not removable. Not click-y. Just something that lets you chew your food, smile in photos, and forget it’s even there. That’s the magic of dental implants.
They’re not a quick fix, though. Replacing a tooth with a dental implant takes time, planning, and a bit of patience. But once it’s in? It’s yours. Let’s walk through what the whole process actually looks like, step by step, without the sugarcoating, and with a few recovery tips from someone who’s been around enough patients to know what really helps.
Starting Off: The Exam and Game Plan
First things first, your dentist isn’t just going to throw a metal post into your jaw. They need to make sure you’re a good fit. That means checking your teeth, gums, bone density, and overall oral health. If your jawbone has shrunk (which can happen when a tooth’s been missing a while), you may need a bone graft first to bulk it back up.
You’ll also have X-rays or scans taken so your dentist can see exactly where the implant will go. They’ll talk through any risks, costs, and the timeline. And be honest with them, about your health, your habits, your concerns. That stuff matters.
If You Need a Bone Graft
Let’s say your jawbone isn’t quite thick enough to hold the implant securely. That’s not the end of the road. It just means a little extra prep work. A bone graft sounds intimidating, but it’s not as dramatic as it sounds. Think of it like adding support beams before building the rest of the structure.
The dentist adds bone material to the area, sometimes using bone from another part of your body, sometimes from a donor, sometimes synthetic. Then, you wait. Healing takes time. Several months, in fact. Your body has to grow around it, make it strong. It’s not fun waiting, but it’s important. Skipping this step could lead to implant failure, and no one wants to go through this whole thing twice.
The Surgery: Where the Implant Goes In
Once your jaw is ready, it’s time for implant placement. This part is surgery, but it’s routine for the dentist. They’ll numb the area (or sedate you if needed), make a small incision in your gum, and carefully drill a spot into the bone to place the implant post. That’s your new artificial tooth root.
You’ll go home the same day, probably feeling a little sore and swollen. Ice packs will be your best friend. Stick to soft foods. Sleep propped up with pillows. Take the painkillers if you need them, but also don’t try to be a hero. Rest is recovery.
Healing: The Part No One Talks About Enough
Now comes the waiting game. As your jaw heals, something pretty amazing happens under the surface. The bone and implant start to fuse together through a natural process called osseointegration. Basically, your body is making the implant part of your jaw. That’s what makes it feel so solid, like a real tooth.
This can take three to six months. Longer, if you had bone grafting. It’s not thrilling, but it’s crucial. Don’t rush it. Use this time to keep your mouth clean, go to your follow-up visits, and take care of yourself. If you smoke, this is your sign to quit, smoking is one of the biggest reasons implants fail.
The Abutment: The Middleman of the Tooth World
Once everything’s healed, you’ll go back to the office for a quick second procedure. This time, the dentist exposes the implant and attaches a small piece called an abutment. It sticks up just a bit above your gumline and acts as the connector between your implant post and your final crown.
The gum tissue will need another few weeks to heal around it. During this time, your dentist might place a temporary healing cap to keep the area clean and shaped just right.
The Crown: Finally, Your Tooth Is Back
This is the day most patients look forward to, getting the crown (or bridge, or denture) placed. Your dentist will take impressions, and a lab will make a custom tooth that matches your other ones in shape, size, and color.
When it’s ready, it gets attached to the abutment, and just like that, your smile is whole again. Most people say they forget it’s even an implant after a few days. You’ll chew normally. Speak without worry. Smile wide.
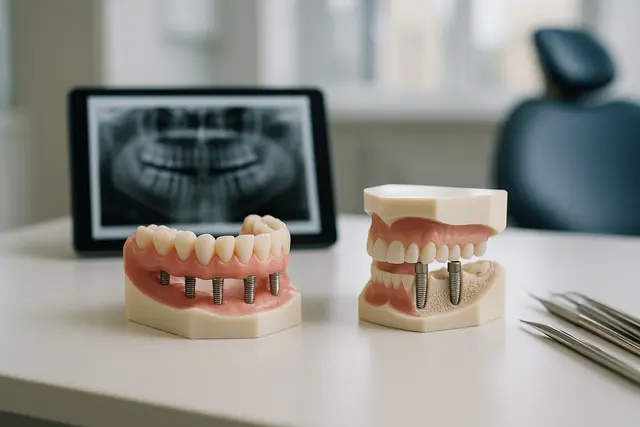
Types of Implants and When They Matter
Most people get what’s called an endosteal implant, which goes directly into the jawbone. But if you don’t have enough bone and don’t want a graft, your dentist may talk to you about subperiosteal implants, which sit on top of the jawbone under the gum.
There’s no one-size-fits-all. That’s why working with the right dental specialist matters. Oral and maxillofacial surgeons, periodontists, they’ve done this a thousand times. They’ll know which type of implant is right for you and how to get it done safely.
Real Recovery Tips from Real Patients
Here’s what people wish they’d known before the procedure:
Don’t plan anything big the day after surgery. You’ll want to rest, trust me.
Have soft foods ready, yogurt, mashed potatoes, smoothies, scrambled eggs.
Keep gauze and ice packs nearby the first 24 hours.
Saltwater rinses are your friend, but skip mouthwash for now.
Stay ahead of the pain. Don’t wait until it’s unbearable to take meds.
Avoid touching the implant with your tongue. It’s tempting, but don’t.
Good oral hygiene doesn’t stop, gently brush the surrounding teeth.
Most importantly: be patient with your body. Healing takes time, and that’s okay.
So... Are Dental Implants Worth It?
If you're someone who hates the idea of something sliding around in your mouth, who’s tired of covering your smile, who just wants to feel normal again when eating corn on the cob, yes, implants are worth it.
They’re not cheap. They’re not instant. But when done right, with proper care, dental implants can last a lifetime. That’s not an exaggeration, it’s what the research shows, and what real patients report, years down the line.
Final Word
This isn’t just about replacing a tooth. It’s about getting a part of yourself back, your bite, your confidence, your comfort. The process can take several months, but at the end of it, you’ve got something strong, stable, and yours.
So if you’re thinking about getting a dental implant, find a dentist you trust, ask all the questions, and go in with your eyes open. The timeline might be long, but the payoff? Absolutely worth it.
How Long Does the Dental Implant Process Take?
The full dental implant process typically takes several months, from initial consultation to final crown placement. This includes healing time after implant surgery (3–6 months), and potentially longer if a bone graft is needed beforehand. While the timeline may vary, the long-term results make the wait worthwhile.
Is the Dental Implant Procedure Painful?
Most patients report only mild discomfort during and after implant surgery. The area is numbed during the procedure, and over-the-counter or prescribed pain medications manage post-op soreness. Swelling and tenderness are normal for a few days, but serious pain is rare when aftercare instructions are followed.
Do I Need a Bone Graft Before Getting a Dental Implant?
You may need a bone graft if your jawbone isn’t thick or strong enough to support an implant. This is common when a tooth has been missing for a while. A bone graft adds structure and stability, but it does add a few months to the timeline to allow for healing.
What Happens After the Implant Is Placed?
After placement, the implant goes through osseointegration, a healing phase where your jawbone fuses with the implant post. Once healed, an abutment is added, followed by your custom crown. With proper care, your new tooth will look, feel, and function like the real thing.
Read Next
Related Posts

Prosthodontics
Implant Supported Dentures Overview
Missing teeth can impact more than just your smile, they can affect your confidence, comfort, and even your diet. Fortunately, modern dentistry offers a solution that’s both secure and natural-looking: implant-supported dentures. This innovative approach blends the stability of implants with the convenience of dentures to create a long-lasting, life-improving upgrade.
5 min read
Oct 29, 2025
Prosthodontics
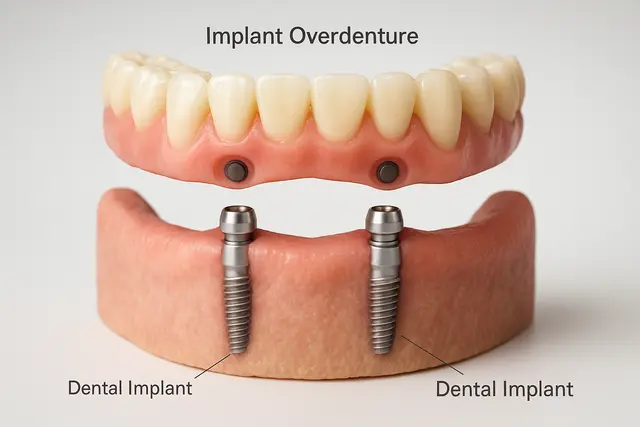
Implant Overdentures Explained: The Hybrid Solution to Missing Teeth
Missing teeth can impact everything from your ability to eat to your self-confidence. While traditional dentures have long been a go-to solution, they often fall short in comfort and stability. Implant overdentures offer a modern alternative that combines the security of dental implants with the convenience of removable dentures, a true upgrade for those looking to reclaim their smile.
6 min read
Oct 29, 2025
Prosthodontics
Implant Retained Dentures Explained
Considering implant-retained dentures? You're not alone. As modern dentistry evolves, more people are turning to this secure, natural-feeling alternative to traditional dentures. This guide will walk you through what they are, how they work, and why they might be the solution you've been looking for.
4 min read
Oct 28, 2025
Don’t have time to research every dentist around you?
See why 30k+ patients trusted us